Microsurgical Varicocelectomy
Why Choose Microsurgical Varicocelectomy?
Microsurgical varicocelectomy (subinguinal microsurgical varicocelectomy) is widely recognized as the most precise, most comprehensive, and most effective method for treating varicocele—with the lowest risk of complications or recurrence.
Unlike higher-level varicocelectomy techniques, the microsurgical approach targets smaller, more numerous, and anatomically complex veins located beneath the external inguinal ring. This allows for meticulous dissection and identification of all problematic veins while preserving surrounding arteries, lymphatic vessels, and the vas deferens.
Hospital-Grade Medical Equipment




Comparison of Varicocele Surgery Techniques
| Surgical Type | Microsurgical Subinguinal | High Retroperitoneal | Traditional Inguinal | Laparoscopic | Scrotal * |
|---|---|---|---|---|---|
| Incision Size | ~1–2 cm | ~5–10 cm | ~5 cm | 3 incisions (~0.5–1 cm each) | — |
| Surgery Time | ~1–1.5 hours | ~1.5 hours | ~40 mins | ~30 mins | — |
| Recurrence/Persistent Symptoms | 0.4% | 15–29% | 2.6–13% | 3–6% | — |
| Complications | Scrotal edema (0.44%), hematoma | Scrotal edema (5–10%), testicular atrophy | Scrotal edema (7.3%), epididymitis, wound issues | Scrotal edema (7–43%), arterial injury, infection | Testicular atrophy, hematoma, edema |
| Special Risks | — | Failure to ligate external veins | Pain from muscle incision, nerve damage | Organ injury, gas embolism, shoulder pain | — |
| Comments | Smallest scar, preserves arteries, lowest recurrence | Larger wound, high recurrence | Shorter surgery, slightly higher recurrence | Allows bilateral repair, preserves arteries | High complication rate; rarely performed |
*Note: Scrotal surgery is rarely performed due to high complication rates and limited supporting data.
Our Surgical Approach: Microsurgical Subinguinal Varicocelectomy
Anesthesia
Traditionally, varicocelectomy is performed under spinal or general anesthesia. At our clinic, we use dual-local anesthesia, allowing patients to remain awake and comfortable. You can even use your phone or headphones during the procedure.
Incision
Whether unilateral or bilateral, only one small incision (~1–2 cm) is made above the scrotum or at the lower pubic area.
Hospital Stay
No hospitalization required. Patients may return home on the same day.
Surgical Procedure
The procedure is performed in the supine position with local anesthesia. Using a surgical microscope, a small incision is made above the scrotum (Figure 1A). The surrounding tissue is separated, and the spermatic cord is isolated (Figure 1B). Dilated veins are carefully dissected and tied with fine microsutures, preserving arteries, nerves, and lymphatic vessels (Figure 1C). No electrocautery is used to prevent thermal damage. The incision is closed with fine sutures (Figure 1D).
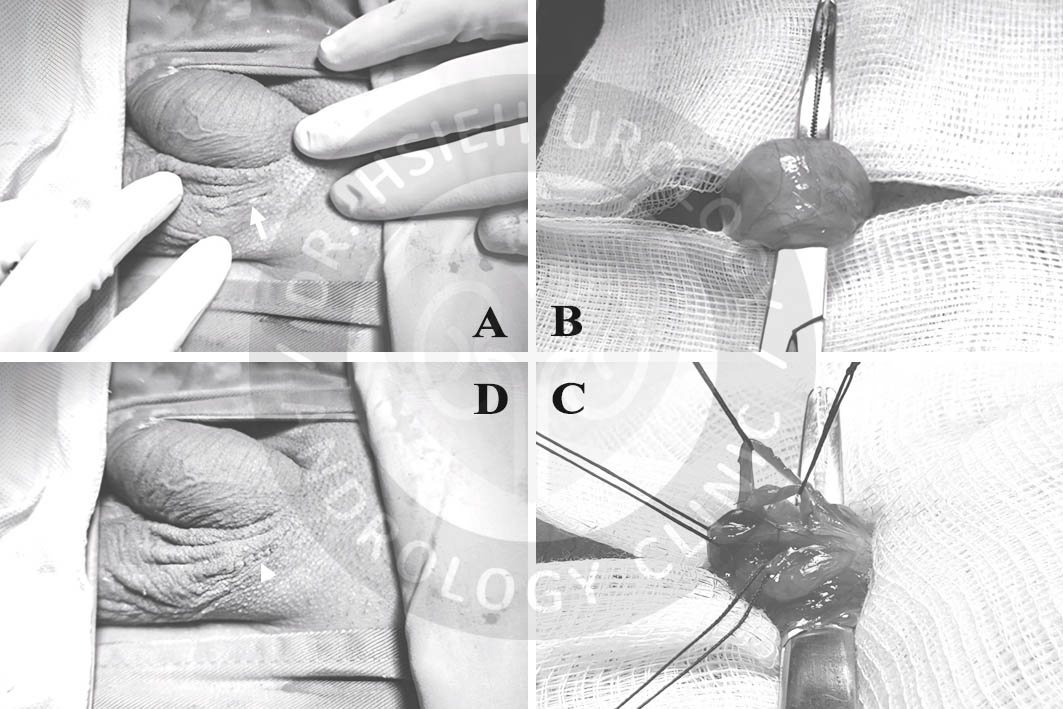
B) Isolation of spermatic cord
C) Ligation of varicose veins with fine sutures
D) Final closure with minimal scarring
Key Benefits at Our Clinic
- Dual-local anesthesia
- Single small incision
- No hospitalization
- No electrocautery—minimal tissue damage
- Microsurgical precision—highest safety
- Reduced risk of complications such as hematoma, chronic pain, infection, or testicular atrophy
Same surgical principles are applied to other procedures including:
- Microsurgical circumcision
- Hernia repair
- Penile vein ligation
- Penile curvature correction
- Penile/testicular prosthesis implantation
- Vasectomy
- Dorsal nerve block surgery
Postoperative Outcomes
- Significant reduction or disappearance of visible/palpable scrotal veins
- Marked improvement in sperm count and motility for patients with poor semen parameters
- Pain relief in 48–90% of patients, especially those with more severe symptoms
- Possibility of sperm presence post-op in patients with azoospermia
- Sperm retrieval success rate increases 2.65x in patients with non-obstructive azoospermia
- Partners’ pregnancy rate increases by 2.39–4.15x post-treatment for oligospermia or idiopathic infertility
- No benefit in subclinical varicocele cases regarding pregnancy outcomes
- Testosterone levels can increase by an average of 34.3 ng/dL, improving hypogonadism symptoms
- May enhance erectile function in patients with ED
- May help delay ejaculation in patients with premature ejaculation
Conclusion
Microsurgical varicocelectomy offers the most effective and safe treatment for varicocele. With low recurrence, minimal incision, and high patient satisfaction, it’s the preferred method among urologists worldwide.
Always consult a specialized urologist to determine the best approach for your condition.
期刊論文
- Hsu GL, Hsieh CH (謝政興), Wen HS, Hsu WL, Chen YC, Chen RM, Chen SC, Hsieh JT. The effect of electrocoagulation on the sinusoids in the human penis (電燒對於人類陰莖海綿體的影響). Journal of Andrology. 25(6):954-9, 2004.
- Hsu GL, Ling PY, Hsieh CH (謝政興), Wang CJ, Chen CW, Wen HS, Huang HM, Einhorn EF, Tseng GF. Outpatient varicocelectomy performed under local anesthesia (局部麻醉門診手術:精索靜脈曲張截除手術). Asian Journal of Andrology. 7(4):439-444, 2005.
- Hsu GL, Zaid UX, Hsieh CH (謝政興), Huang SJ. Acupuncture assisted local anesthesia for penile surgeries (針灸輔助局部麻醉下施行陰莖手術). Translational Andrology and Urology. 2(4):291-300, 2013.
- Hsu GL, Hsieh CH (謝政興), Chen HS, Ling PY, Wen HS, Liu LJ, Chen CW, Chua C. The advancement of pure local anesthesia for penile surgeries: can an outpatient basis be sustainable (純粹局部麻醉施行陰莖手術的新進展)? Journal of Andrology. 28(1):200-205, 2007.
書籍著作
- Geng-Long Hsu (許耕榕)、Cheng-Hsing Hsieh (謝政興). 書名:A LABORATORY MANUAL FOR POTENCY MICROSURGERY (性功能顯微手術實驗訓練手冊). 許耕榕、謝政興,編輯.
參考文獻
- 2020台灣泌尿科醫學會(TUA)泌尿科治療指引
- Salonia A, Bettocchi C, Capogrosso P, et al. Premature ejaculation. In. EAU Guidelines on sexual and reproductive health. pp. 64-73, 2023
- Hsu GL, Hsieh CH (謝政興), Wen HS, Hsu WL, Chen YC, Chen RM, Chen SC, Hsieh JT. The effect of electrocoagulation on the sinusoids in the human penis (電燒對於人類陰莖海綿體的影響). Journal of Andrology. 25(6):954-9, 2004.
- Lotti F, Corona G, Mancini M, et al. The association between varicocele, premature ejaculation and prostatitis symptoms: possible mechanisms. J Sex Med. 2009;6(10):2878–2887.
- Abu El-Hamd M, Abdel Hameed FA. The Role of Varicocelectomy on Patients with Premature Ejaculation and Varicoceles. 2016;3(4):121–125. Journal of Integrative Nephrology and Andrology.
- Zohdy W, Ghazi S, Arafa M. Impact of varicocelectomy on gonadal and erectile functions in men with hypogonadism and infertility. J Sex Med 2011; 8: 885–93.
- Ji B, Jin XB. Varicocele is associated with hypogonadism and impaired erectile function: a prospective comparative study. Andrologia. 2017;49(6). doi:10.1111/and.12683, 10.1111/and.12683
