The purpose of anesthesia during surgical procedures is to ensure that the patient does not experience pain or any awareness while the operation is being carried out. This allows for a successful completion of the surgery without any discomfort or symptoms after the procedure, and an immediate recovery to the preoperative state. Anesthesia carries certain risks, mainly associated with the patient’s underlying conditions (such as cardiovascular disease, poor lung function, or diabetes), inherent conditions (such as old or young age), and different surgical approaches. Therefore, a preoperative assessment should be carried out, taking into account the patient’s age, weight, medical history, surgical site, and different medical conditions, to choose an appropriate anesthesia method and reduce the potential risks associated with anesthesia.
Local anesthesia can be divided into two categories: injection and infiltration. In clinical practice, injection-type local anesthesia is commonly used for outpatient surgeries. Prior to surgery, there is no need for fasting or catheterization. An anesthetic is injected near the surgical site to block nerve transmission and achieve painlessness during surgery. However, patients may still feel movement or heaviness in the surgical area, but they will not experience pain. Patients are conscious throughout the surgery and the effects of local anesthesia gradually wear off over several hours. Additional doses of anesthesia can be administered if necessary. On the day of the surgery, patients can take oral antibiotics and painkillers and return home without being hospitalized.
Local anesthesia is suitable for small and superficial surgical sites. If the risk of half-body or general anesthesia is high during patient evaluation, and the technique of local anesthesia is skillful, local anesthesia can be used instead to reduce the risk of anesthesia and to perform relevant surgery. Local anesthesia is safe and has the lowest risk and almost zero mortality compared to other anesthesia methods. It is simple and convenient to use, has a small affected area, works quickly, has fewer side effects, and has a shorter duration of action. However, if the lesion is too deep or too large or if there is inflammation or swelling, local anesthesia may not be suitable, and special attention must be paid to whether the patient has a history of allergy to anesthesia drugs.
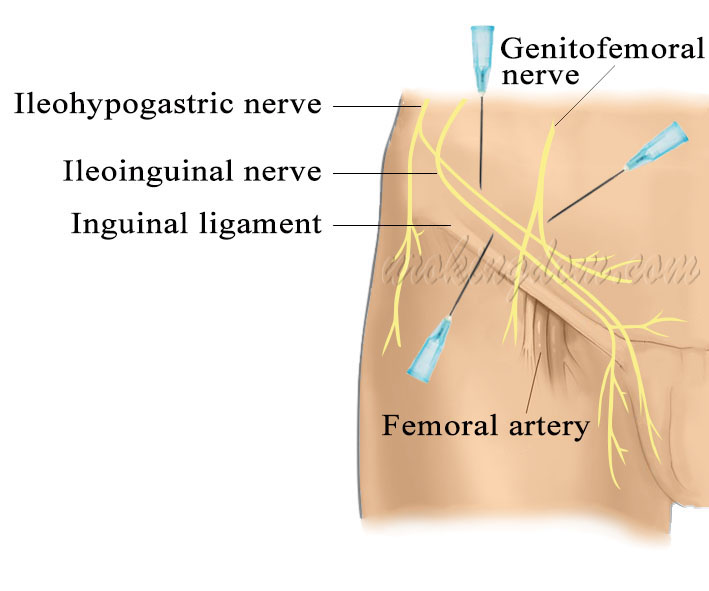
An innovative dual local anesthesia approach is used to assist in microscopic inguinal hernia repair surgery. A local anesthetic solution containing a small amount of adrenaline and lidocaine is used for local anesthesia injection. This includes the blockage of the iliohypogastric nerve, the genital branch of the genitofemoral nerve, and the ilioinguinal nerve in the vicinity of the inguinal canal (see Figure 1), which completes the subcutaneous tissue anesthesia and prolongs the effective anesthesia time for 4-6 hours or longer. The surgery is performed painlessly and with consciousness. The surgeon can perform precise and meticulous surgery without time pressure, reducing the potential complications and postoperative pain and enhancing the quality of surgery. Patients can return home on the same day after surgery.
Regional anesthesia, also known as spinal anesthesia, includes spinal anesthesia and epidural anesthesia. The anesthetic is injected into the spinal cord or epidural space to achieve nerve blockade and to stop pain during surgery. The patient is conscious during the process and this method is typically used for surgery in the lower abdomen or lower limbs, such as urological, gynecological, or hernia surgery. After injection of the anesthetic, the height of the anesthesia site is not easily adjustable. The duration of anesthesia usually lasts for about 2-3 hours, which is not suitable for longer surgeries. Epidural anesthesia is more technically challenging and is suitable for longer surgeries. It has less impact on respiratory function and blood pressure changes and can also be used for postoperative pain relief. Most hernia surgeries use regional anesthesia and require hospitalization and care.
General anesthesia includes endotracheal general anesthesia, general anesthesia with laryngeal mask, and intravenous general anesthesia. Anesthetic gases or injectable drugs are used to help patients enter a sleep state and undergo surgery while in a state of muscle relaxation with the help of medical instruments and equipment to aid in breathing. Endotracheal general anesthesia and general anesthesia with laryngeal mask are usually used for major surgeries with longer surgical times and special postures, such as those involving the head and neck, chest, and abdomen. The risks of anesthesia are usually higher than other anesthesia methods. Intravenous general anesthesia mainly uses intravenous injection of anesthetic drugs to achieve a sedative and analgesic effect during surgery. However, longer surgeries require more anesthetic drugs, and the maintenance of the airway is not as good as the other two types of general anesthesia mentioned above, which may affect patient recovery time and increase anesthesia risk. Therefore, it is mainly used for shorter surgeries. Laparoscopic or Davinci hernia surgeries must use endotracheal general anesthesia and require hospitalization and care.

