骨盆底功能障礙是一種影響女性骨盆器官正常功能的疾病,包括腸道、泌尿道、骨盆支撐和性功能等各方面的障礙。陰道分娩和相關創傷被認為是骨盆底損傷的主要致病原因。特別的生產因素,例如巨大胎兒和器械助產,可能造成更大的骨盆底損傷。此外,更年期相關的荷爾蒙變化和結締組織特性,與骨盆底症狀的發生亦有相關。 膀胱過動症候群(Overactive bladder syndrome, OAB)是一種常見的骨盆底功能障礙,國際尿失禁防治協會(ICS)將膀胱過動症定義為「尿急,可能有急迫性尿失禁,通常伴隨發生頻尿及夜尿」。目前膀胱過動症候群的第一線治療方法是行為治療,包括骨盆底肌肉自主運動(凱格爾運動)、生物回饋、電刺激和電磁刺激治療等。
高強度聚焦電磁技術
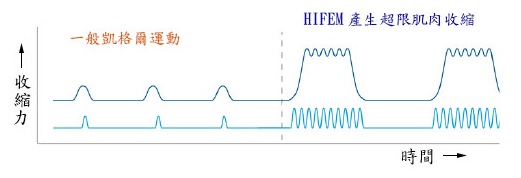
高強度聚焦電磁技術(High-intensity focused electromagnetic technology, HIFEM)應用法拉第的電磁感應定律,由此產生即時變動的磁場感應電流,用於刺激中樞和周圍神經系統,誘導神經去極化,導致骨盆肌肉收縮並且調控第2節至第4節(S2-S4)的薦椎神經反應。由於此一特性,高強度聚焦電磁技術已被應用於治療各類型的尿失禁及膀胱過動症。在治療過程中,主要是刺激會陰部神經,重複的刺激活化末端運動神經纖維會增強骨盆底肌肉(包括尿道括約肌)的張力和耐力,改善尿失禁;並且透過中樞神經防衛反射,抑制膀胱逼尿肌收縮,改善頻尿、急尿等膀胱過動症的相關症狀。與其他形式的骨盆肌肉強化治療類似,高強度聚焦電磁技術使尿道橫紋括約肌產生肥大效應,亦有助於抑制膀胱的急尿感。
由於高強度聚焦電磁技術沒有直接活化C型神經纖維和皮膚的感覺受體,不會造成疼痛不適,比傳統的電刺激更舒適。因此高強度聚焦電磁技術於1998年獲得美國食品藥物管理局批准核可用於治療尿失禁等醫療用途。
磁波椅 – 肌緊椅
最新的UI CUBE肌緊椅(圖二)採用目前最高強度(2.5特斯拉)聚焦電磁技術的治療裝置,其結構由一個發電機和一個內部安裝的圓形線圈所組成。相較於一般推薦應用的凱格爾運動,磁波椅儀器裝置應用高強度聚焦電磁技術,能達到更有效率、更加強化的骨盆底肌肉收縮訓練。接受 20分鐘的治療可以達到12,000次凱格爾運動的效果,將凱格爾運動的益處最佳化,並且透過強化盆底肌肉來增加自主肌肉收縮力量,使尿道橫紋括約肌產生肥大效應,有助於抑制膀胱的急尿感;並且經由中樞神經防衛反射,抑制膀胱逼尿肌收縮,改善膀胱過動症候群的相關症狀。

參考文獻
- Frigerio, M.; Barba, M.; Cola, A.; Marino, G.; Volontè, S.; Melocchi, T.; De Vicari, D.; Maruccia, S. Flat Magnetic Stimulation for Stress Urinary Incontinence: A Prospective Comparison Study. Bioengineering 2023, 10, 295.
- Braga A, Castronovo F, Caccia G, Papadia A, Regusci L, Torella M, Salvatore S, Scancarello C, Ghezzi F, Serati M. Efficacy of 3 Tesla Functional Magnetic Stimulation for the Treatment of Female Urinary Incontinence. J Clin Med. 2022;11(10):2805.
- Lukanovi´c, D.; Kuniˇc, T.; Batkoska, M.; Matjašiˇc, M.; Barbiˇc, M. Effectiveness of Magnetic Stimulation in the Treatment of Urinary Incontinence: A Systematic Review and Results of Our Study. J. Clin. Med. 2021, 10, 5210.
- Duncan D, Dinev I. Noninvasive Induction of Muscle Fiber Hypertrophy and Hyperplasia: Effects of High-Intensity Focused Electromagnetic Field Evaluated in an In-Vivo Porcine Model: A Pilot Study. Aesthet Surg J. 2020;40(5):568-574.
- Samuels JB. HIFEM Technology – The Non-Invasive Treatment of Urinary Incontinence. 2018; Presented at 38th American Society for Laser Medicine and Surgery Annual Conference. on “Energy-based Medicine and Science”, April 11-15, 2018
- Aragona SE, Mereghetti G, Lotti J, Vosa A, Lotti T, Canavesi E. Electromagnetic field in control tissue regeneration, pelvic pain, neuro-inflammation and modulation of non-neuronal cells. J Biol Regul Homeost Agents. 2017;31(2 Suppl. 2):219-225.
- Fergany LA, Shaker H, Arafa M, Elbadry MS. Does sacral pulsed electromagnetic field therapy have a better effect than transcutaneous electrical nerve stimulation in patients with neurogenic overactive bladder?. Arab J. Urol.. . 2017;15(2):148-152.
- Lo, T.S.; Tseng, L.H.; Lin, Y.H.; Liang, C.C.; Lu, C.Y.; Pue, L.B. Effect of extracorporeal magnetic energy stimulation on bothersome lower urinary tract symptoms and quality of life in female patients with stress urinary incontinence and overactive bladder. J. Obstet. Gynaecol. Res. 2013, 39, 1526–1532.
- Abrams, P.; Cardozo, L.; Fall, M.; Griffiths, D.; Rosier, P.; Ulmsten, U.; Van Kerrebroeck, P.; Victor, A.;Wein, A. The standardization of terminology of lower urinary tract function: Report from the standardization sub-committee of the International Continence Society. Neurourol. Urodyn. 2002, 21, 167–178.
- Galloway NT, El-Galley RE, Sand PK, Appell RA, Russell HW, Carlan SJ. Extracorporeal magnetic innervation therapy for stress urinary incontinence. Urology. 1999 Jun;53(6):1108-11.
- Fall, M.; Lindström, S. Functional electrical stimulation: Physiological basis and clinical principles. Review article. Int. Urogynecol. J. 1994, 5, 296–304. Barker, A.T.; Freeston, I.L.; Jalinous, R.; Jarratt, J.A. Magnetic stimulation of the human brain and peripheral nervous system: An introduction and the results of an initial clinical evaluation. Neurosurgery 1987, 20, 100–109.
